Key points
• Ankylosing spondylitis is a type of arthritis that affects the spine
• There’s no cure, however it can be managed with medication and lifestyle changes
• The most important thing you can do is regular exercise, which helps to keep your spine mobile and flexible
Summary
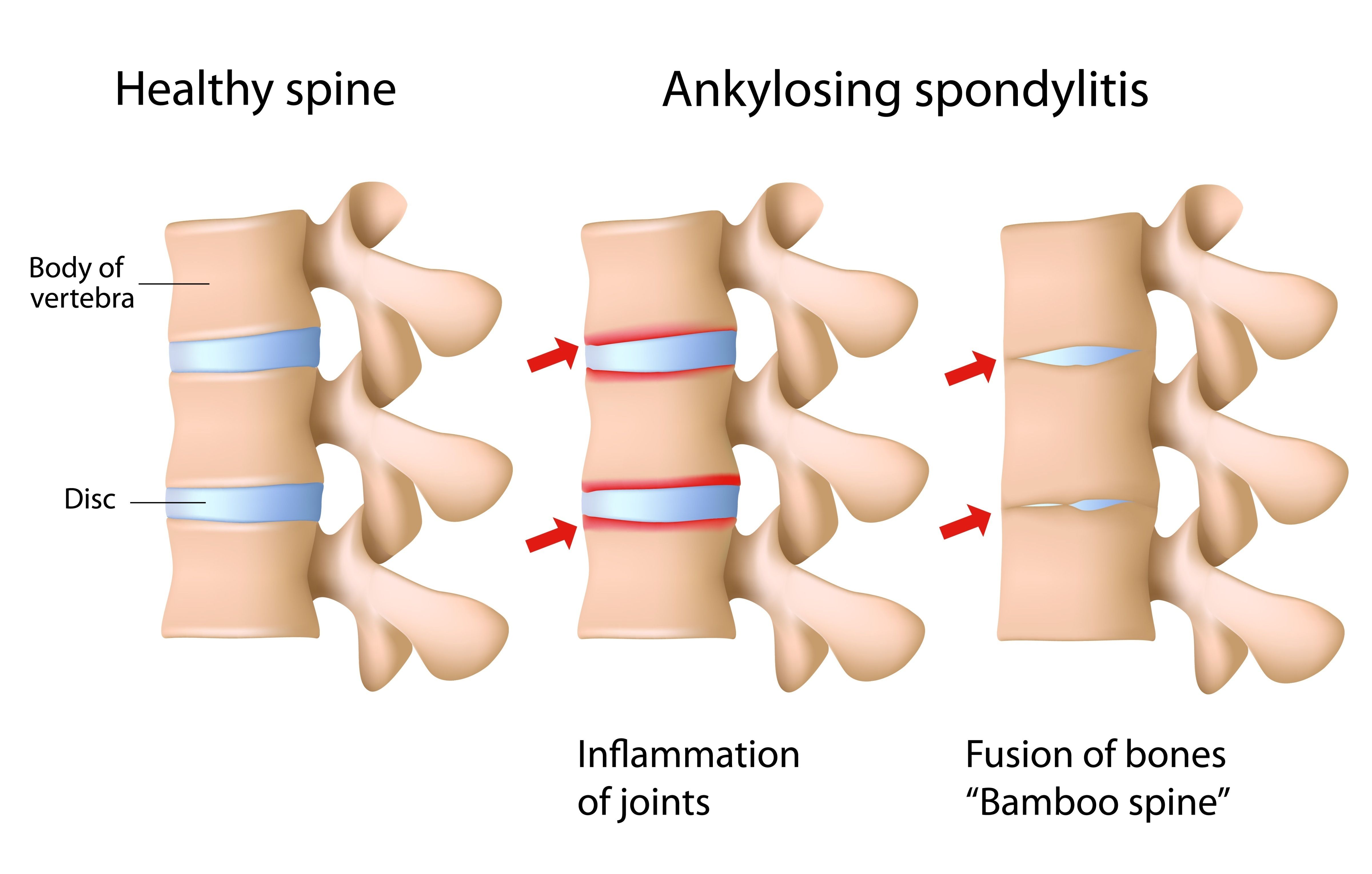
Ankylosing spondylitis (AS) is a type of inflammatory arthritis that targets the joints of the spine. It first affects the sacroiliac (SI) joint, where the spine attaches to the pelvis, and then starts to affect other areas of the spine. The hips and shoulders can be affected, as can the eyes, skin, bowel and lungs. Symptoms of AS include back pain, stiffness and reduced mobility in the spine.
AS affects men more often than women and usually appears between the ages of 15 and 45 years. While there’s currently no cure for AS, there are many things you can do to help control your symptoms.
AS is an autoimmune disease. That means that it occurs as a result of a faulty immune system. Instead of identifying foreign bodies (e.g. bacteria, viruses) and attacking them to keep you healthy, your immune system mistakenly attacks healthy tissue in and around your joints causing ongoing inflammation and pain.
In AS, as a result of this inflammation, new bone may grow around the joints in the spine. This can lead to permanent stiffness in the back and neck of some people with AS.
In severe cases, this extra bone can fuse the bones of the spine together. This used to be common, but now can usually be prevented by starting appropriate treatment as early as possible.
Symptoms
The symptoms of AS vary from one person to the next, but they’re usually worse after rest and relieved with exercise.
The most common symptoms are:
-
pain and stiffness in the back, buttocks or neck, especially in the morning or if you’ve been inactive for a period of time
-
pain in tendons (which connect muscles to bones) and ligaments (which connect bones to each other), often felt as pain at the front of the chest, back of the heel or underneath the foot
-
fatigue (extreme tiredness).
Symptoms may change from day to day. At times your symptoms (e.g. pain, fatigue, inflammation) can become more intense. This is a flare. Flares are unpredictable and can seem to come out of nowhere.
Cause
The exact cause of AS is unknown. Genes are thought to play a role. You’re more likely to get AS if you have a history of it in your family.
Studies show that almost nine out of ten people with AS have the gene called HLA-B27. However eight per cent of the general population, including people without AS, have this gene.
Since just having this gene doesn’t automatically lead to the development of AS, other factors are thought to be involved.
Researchers currently think that exposure to certain environmental triggers can lead to the development of AS in people with the gene. But these triggers are unknown.
Diagnosis
Early diagnosis is important so that treatment can be started as soon as possible. AS may be diagnosed using a number of tests including:
-
medical history physical examination scans such as x-ray, CT (computed tomography), MRI (magnetic resonance imaging)
-
blood tests genetic testing.
These tests are generally organised by your doctor or rheumatologist (a doctor who specialises in muscle, bone and joint conditions). They will explain what the tests are looking for and what the results mean.
Treatment
There’s no cure for AS, so treatment aims to manage your pain, reduce your risk of complications and improve your quality of life. It will be tailored to your specific symptoms and the severity of your condition.
Medication
Medications used to treat AS include:
-
pain relievers (or analgesics) - for temporary pain relief
-
non-steroidal anti-inflammatories (NSAIDs) - control inflammation and provide pain relief
-
corticosteroids - to quickly control or reduce inflammation
-
disease-modifying anti-rheumatic drugs (DMARDs) - control your overactive immune system
-
biologics and biosimilars (bDMARDs) – are biological disease-modifying drugs that work to control your immune system, but in a much more targeted way.
Self-management
There are many things you can do to help yourself:
-
learn more about your condition – knowing as much as possible about your AS means that you can make informed decisions about your healthcare and play an active role in managing it.
-
exercise and stay active as much as possible – talk with a physiotherapist or an exercise physiologist for specific advice.
-
get up and move if you’ve been sitting or standing in one position for long periods at a time (e.g. at work, while travelling).
-
stay involved – in your usual home activities, work, leisure and social activities. Social connections are extremely important.
-
be aware of your posture – when sitting, standing and even lying down. Your body should be in correct alignment but also loose and flexible.
-
eat a healthy, well balanced diet for general good health.
-
manage your stress – it can aggravate your symptoms and make you feel worse.
-
acknowledge your emotions – it‘s natural to feel overwhelmed when you’re diagnosed with AS. You may feel scared, anxious, frustrated, sad or angry. It’s important to acknowledge these feelings and get help if they start affecting your daily life. Your doctor can provide you with information about support that’s available.
-
seek support from others – you might find it helpful to contact the Ankylosing Spondylitis Group of Victoria and speak to other people who have AS and know what you’re going through. Contact us for information and contact details.
Things to remember
-
Ankylosing spondylitis is a type of arthritis that affects the spine
-
There’s no cure, however it can be managed with medication and lifestyle changes
-
The most important thing you can do is regular exercise, which helps to keep your spine mobile and flexible
Where to get help
-
Your doctor
-
Physiotherapist
-
Exercise physiologist
-
MOVE muscle, bone & joint health
National Help Line: 1800 263 265
How we can help
Need medical information regarding your condition and commonly prescribed treatments? Or assistance navigating the health, disability and social services systems? Contact our nurses on the Help Line on 1800 263 265 or email helpline@move.org.au.
Interested in finding out about our upcoming webinars and seminars and other events? Click here to learn more.
More to explore
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.




